BRATTLEBORO — For 50 years, Rescue Inc. has lived up to its name as a provider of emergency services in southeastern Vermont.
These days, though, Rescue itself is in urgent need of some relief.
Windham County legislators gathered on Jan. 18 at the ambulance service's Brattleboro headquarters to get the latest on what Operations Chief Drew Hazelton is calling a “financial crisis.”
There are increasing demands for complex medical services, and the state's Medicaid reimbursement rates - which haven't changed since 2008 - are forcing ambulance administrators to write off hundreds of dollars every time they respond to a call.
Lawmakers didn't have to look far to see the impacts of that situation. Hazelton said that, as of the day of the legislative meeting, budget cuts had forced him to reduce staffing and to order Rescue's administrative and training officers to respond to routine medical calls.
“We need staffing. We need equipment. We need education. It all starts off with money,” Hazelton said. “We can't do any of it unless we can pay our bills. We need to get reimbursed at a rate that at least covers our costs.”
Hazelton was joined at the session by Heidi Taylor, business administrator at Wilmington-based Deerfield Valley Rescue. The two supplied a handout to visiting lawmakers that included quotes and data from rescue services based in Richmond, Barre City, Newport, Lyndon, and St. Michael's College.
The message was clear.
“This is not unique to Rescue. It's not unique to Deerfield Valley,” Hazelton said. “This is a statewide problem.”
The problem, on one hand, is the changing business of running an ambulance service. Aided by props that included a dummy, a flat-screen television, and an array of medical equipment with accompanying price tags, Rescue Inc. administrators showed legislators how their costs are climbing.
Items on display included a $160,000 ambulance, a $40,000 cardiac monitor, and an $11,000 ventilator.
“This is not first aid like it was when EMS started. The expectation of the public is that they're getting emergency room or ICU-level treatment at their house,” Hazelton said. “That's also the expectation of the hospitals, because our health care requires us to (transport) patients from smaller community hospitals to specialty centers.”
While the rising cost of health care is a nationwide issue, officials said there are aggravating factors at play in the Green Mountain State. The state's well-publicized heroin problem and its overburdened mental-health system are two prime examples, and paramedics are on the front lines for both.
“We've watched our mental health/substance abuse population double in two years,” Hazelton said.
“We've also noticed, in our coverage area here in Brattleboro, that the heroin is spreading,” he added. “We didn't used to see a lot of heroin overdoses at our Townshend office. Now, it is at least a weekly occurrence.”
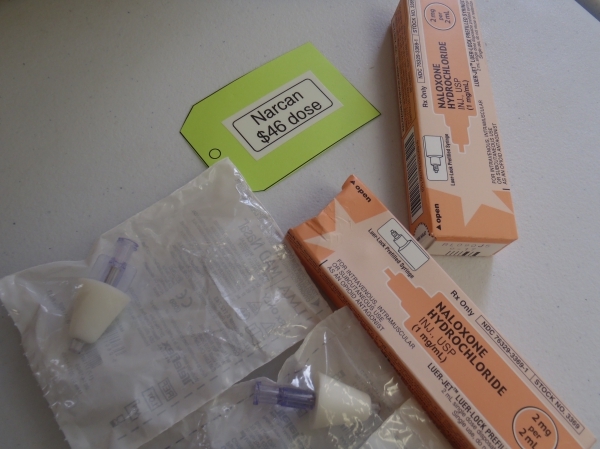
Increasing numbers of overdose and mental-health calls are accompanied by an increased threat of violence and the need for specialized equipment, officials said. That includes the opiate antidote Narcan, which allows medics to quickly “wake up” an overdose victim.
At one point, Narcan “was so cheap, we used to practice with it,” Hazelton said. But times have changed. Deerfield Valley Rescue says its price for a single dose of the drug has jumped from $16.95 in 2014 to $45.99 this year.
Neither Medicare nor Medicaid reimburses medics for the Narcan they use. As a matter of fact, “there are no reimbursements for medications,” Hazelton said. “It doesn't matter if it's a cardiac arrest or an overdose. All medications come straight out of our pocket.”
There's also no place in Vermont's health care reimbursement system for patients that aren't transported via ambulance. While Rescue's medics sometimes can treat a person in his or her home in order to avoid a trip to the emergency room, “we only get paid if we move patients,” Hazelton said.
That puts more pressure on fund-raising, such as the truck raffle that Rescue Inc. held last year. But for coverage of day-to-day expenses, medics look mostly toward Medicare and Medicaid reimbursements.
And they argue that those payments are insufficient to sustain a busy rescue organization. Taylor said the federal Medicare program pays 80 percent of what the government says are “reasonable and customary costs” for an ambulance run.
Things are worse from the state's end of the equation, as Medicaid pays only 42 percent of what the federal government would pay, Taylor said. And that's bad news for outfits like Rescue Inc., as federal health care changes have dramatically boosted the number of patients on Medicaid.
“Here in Brattleboro, we've watched our Medicaid population go from 18 to 35 percent,” Hazelton said. “We can't cost shift it to anybody else ... our private insurance pool is now less than 10 percent of the calls we go on.”
The bottom line: “Right now, we're losing an average of about $350 per Medicaid call that we go out on,” Hazelton said.
He's not alone in such sentiments. Literature from the Vermont Ambulance Association includes this quote from Richmond Rescue: “It would take us four Medicaid patient transports to equal one transport of a commercially insured patient. Each year, we write off tens of thousands of dollars due to the low Medicaid reimbursements.”
At the Jan. 18 meeting, Taylor also pointed out that first responders can't elect to take some patients and not others for financial reasons.
“When you dial 911, we don't ask what your insurance is. We come,” she said.
As a result, ambulance services' budgets are strained to the breaking point: Hazelton said he is now working with Rescue Inc.'s board to cut $200,000 in expenses. And with municipal contributions to Rescue set far in advance, there's no way to seek additional money from towns to help cover the current year's expenses.
“If the call volume and the current mix of insured and uninsured patients doesn't change, then the (staffing) change that we made ... will keep our budget balanced through the end of the fiscal year,” Hazelton said.
“In the meantime, we are working to try to maximize every dollar we can and fundraise more,” he added.
In cash-strapped Vermont, it's no small thing to suggest boosting the state's Medicaid reimbursements.
Gov. Peter Shumlin's fiscal year 2016 proposal to do so via a payroll tax was rejected. In his Jan. 21 budget address for fiscal 2017, Shumlin proposed levying a new, 2.35 percent provider tax on independent doctors and dentists in order to help fund a small increase in Medicaid reimbursements.
“Vermont should not be the state that signs people up for Medicaid just to turn our backs on them,” Shumlin wrote in his prepared budget remarks. “Vermont should not be the state who begs our doctors and nurses to take care of folks on Medicaid just to turn their backs on them. That's not leadership and it's not good government.”
The Windham County legislators in attendance at the Jan. 18 meeting brainstormed a few ideas to help paramedic services, but there were no easy solutions pitched during the nearly two-hour session.
Rep. Ann Manwaring, D-Wilmington, suggested that Vermont's ambulance services need to do a better job of letting policymakers know about how their duties have evolved and how that has led to their current predicament.
“Get a different conversation going than just, 'I don't have enough money,'” Manwaring said. “We're all done with, 'I don't have enough money,' conversations in the Statehouse. No one has enough money.”
“In some ways, the message about how you have become a different type of functioning entity has not really gotten out there into the world,” she added.
The legislators offered to help get that point across, and Hazelton said such receptiveness would be a welcome change. Without some sort of solution, he warned, there will be consequences.
“At the end of the day, our local tax base is going to get billed back the difference. It's going to end up on the local property tax,” Hazelton said. “Or this level of service, whether it be for emergencies or inter-facility transfers, is going to stop.”