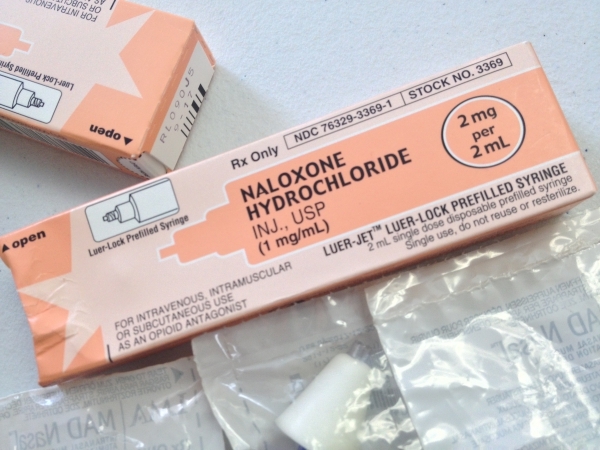
BRATTLEBORO — It's been more than two years since Vermont, in the midst of an opiate crisis, began distributing free doses of the overdose-reversal drug naloxone.
And recently released state statistics back up what Gov. Peter Shumlin declared in his Jan. 21 budget speech: Naloxone, also known under the brand name Narcan, “has saved hundreds of lives” during that time.
But it's also become clear that there are complexities associated with attempting to quickly rouse an overdose victim. For one thing, officials warn that some opiates now on the street are so strong that multiple doses of naloxone are needed to ensure that an “awakened” patient remains conscious.
Also, some medics are seeing increasing numbers of assaults by those who have regained consciousness after an overdose.
It doesn't seem to be happening everywhere in the state, but assaults have been reported by the Vermont Ambulance Association and by medics at Brattleboro's Rescue Inc.
“This is not uncommon. Last year, we had a lost-work injury that was almost six months due to an overdose assault,” Drew Hazelton, Rescue Inc. chief of operations, told state lawmakers during a January meeting in Brattleboro.
“When (overdose victims) come off a high abruptly with Narcan, they can become violent,” Hazelton said. “Quite often, they become violently ill. And it's not a pleasant experience.”
To be sure, no one is calling for decreased use of naloxone because of such issues. While the anti-overdose drug is just one way to combat the complex problems of addiction, naloxone has been praised as a fast-acting, easy-to-administer antidote in life-or-death situations.
“If you die of an overdose, you don't get a chance for treatment,” said Michael Leyden, who manages the state Department of Health's naloxone pilot program.
That pilot program began in December 2013, and there currently are 10 sites around the state where residents can pick up free “overdose rescue kits” containing two doses of nasally administered naloxone. More information is available at healthvermont.gov/adap/treatment/naloxone.
Those sites have been relatively busy. In a report assessing the pilot program from December 2013 through September 2015, officials said 6,989 doses of naloxone have been dispensed - 4,182 doses to new clients and 2,807 doses to returning clients.
The report says 36 percent of those new clients had personally experienced an overdose, while 63 percent said they had witnessed an overdose. Among those who had overdosed, heroin was by far the most-frequent culprit, though overdoses on alcohol, benzodiazepines, cocaine, methadone, and suboxone also were reported.
While the Health Department is keeping close tabs on who receives the naloxone kits, officials say it is harder to gather specific data on how those kits have been used. Based on reports from those who have requested refills, the department says 233 clients have used the drug 401 times in response to perceived overdoses.
Because of such statistics, Shumlin's proposed fiscal year 2017 budget includes $200,000 to continue the naloxone pilot program beyond the end of this fiscal year, when it is due to expire.
Along with the increasing availability of naloxone among the general public, a growing number of emergency responders also are carrying the drug.
For example, Burlington police began carrying naloxone in January, joining that city's firefighters and health-service providers. And Vermont State Police have been carrying the anti-overdose medication since 2014.
Police officers have not been using the drug very often, however. State Police spokesman Scott Waterman said there were just six naloxone deployments by troopers in 2015, and he provided statistics showing that the drug was used only six times by four other Vermont law enforcement agencies last year.
One reason for such low numbers, Waterman said, is the presence of emergency medical responders at most overdose scenes.
In Brattleboro, Rescue Inc. personnel are intimately acquainted with naloxone - and its effects on those who have overdosed. While not questioning the drug's effectiveness, Hazelton let local lawmakers know that his staff frequently must deal with violent outbursts from revived overdose victims.
“When you're in a bathroom with somebody who's unconscious and suddenly comes up swinging, there's no place for you to go,” Hazelton said during a Jan. 18 session at the emergency provider's Canal Street headquarters.
Hazelton said the reaction is due in part to the uncertainty and anger of addicts who are waking up. With medics in uniform, “we all look like cops because we're there standing over them,” he said.
The experience is not unique to Brattleboro.
“That does happen, so we have had injuries in the past,” said Jim Finger, who leads Rutland Regional Ambulance Service and also serves as Vermont Ambulance Association president.
“It's a dangerous job at times,” Finger added. “But the drug problem is here, and it's everywhere.”
The frequency of such incidents is difficult to pin down. Hazelton indicated that assaults by overdose victims can be a weekly occurrence, but there were no ambulance association or statewide statistics available.
“We haven't detected it as an issue from the pilot program perspective thus far,” Leyden said. “It's certainly not something that's risen to our level of awareness.”
But Leyden is well aware that overdose victims can become agitated when revived, noting that naloxone is a “pretty powerful crowbar” for pulling patients back to consciousness and immediately into severe withdrawal.
That's one reason why state officials, in an educational handout about using naloxone, urge everyone who believes they are witnessing an overdose to call 911 first - even before administering rescue breathing or naloxone.
Pilot program data, however, show that's not been happening in a majority of cases: Only 28 percent of those who reported using naloxone to counteract an overdose said they called 911.
“Really, we want to get (overdose victims) into the medical system,” Leyden said. “That doesn't happen with the frequency that we'd like, but that's a hard behavior to change.”
The state's rescue kit instructions also counsel those who revive a patient to “remind the person that naloxone will wear off in a little while, and they will stop feeling dope sick.”
That's meant to help calm patients who “can feel pretty horrible coming out of that - they can be frightened and be unaware of what's going on around them,” Leyden said.
The reference to naloxone wearing off, however, also hints at another complication associated with the drug - the fact that one dose might not be enough to save a life.
“Narcan is a great drug, but it (sometimes) doesn't last as long as the drugs that are on the street right now,” Hazelton said. “So we're not getting away with one dose of Narcan.”
Some patients are “waking their buddy up with the Narcan that they were given, and 10 minutes later, they're not breathing again because the Narcan wears off long before the drugs,” he added. “There's a reason why we carry boxes and boxes and boxes of it.”
The state's pilot program statistics illustrate the same issue. Thirty-one percent of those who used naloxone said they had deployed two doses, and another 8 percent said three or more doses were necessary.
Leyden said more-powerful opiates - such as heroin that's been combined with the painkiller fentanyl - can necessitate multiple doses of the anti-overdose drug. But he said it's difficult to generalize about how much naloxone will be needed in any given case.
“Naloxone as a drug is relatively short-acting. Your body metabolizes the drug, and it wears off within a certain amount of time,” Leyden said. “Depending on the opioid and when you took it, the naloxone can wear off and the overdose symptoms can come back.”
For medics arriving at an overdose scene, it's sometimes difficult to tell initially what a patient took and when. That's why emergency responders lean so heavily on naloxone and say they will continue to do so.
“It's very important that we have it,” Finger said. “There's no doubt about it, that it does its job.”