BRATTLEBORO — This was supposed to be a simple story about Atul Gawande - a New England surgeon turned author of the nationally best-selling book Being Mortal - born of an unexpected meeting in the fall of 2017.
“The conversation I felt like I was having was, do we fight, or do we give up?” I heard him say on public radio the weekend before. “And the reality was that it's not 'Do we fight, or do we give up?' - it's 'What are we fighting for?' People have priorities, besides just surviving no matter what. You have reasons you want to be alive. What are those reasons?”
Then my father was diagnosed with fast-spreading cancer and died soon after, turning this into something personal.
* * *
Most people don't want to think - let alone talk about - mortality, starting with health-care providers who often view saving lives as the only measure of success. That's why Gawande, believing physicians and patients need to acknowledge and address reality, wrote Being Mortal: Medicine and What Matters in the End.
“When I turned it in,” he recalls, “my agent said, 'It's an important book, but I have no idea how commercial this is. Who's going to buy a death book coming out at Christmas?'”
Surprisingly, seemingly everyone.
Two months after its 2014 publication, Being Mortal had sold more copies than the author's three previous best sellers combined. Five years later, it remains on The New York Times top-15 paperback nonfiction sales list.
I was not one of those buyers. Stumbling on Gawande's radio interview two years ago, I didn't know I'd be sitting next to him at a journalism roundtable that week.
I figured we had little in common, what with my home in small-town Brattleboro and his in big-city Boston, my single paycheck versus his juggling jobs at The New Yorker, Harvard Medical School, and a new health-care venture formed by Amazon, Berkshire Hathaway, and JPMorgan Chase.
“A lot of that,” he told me of his life, “is dependent on being incredibly ruthless about prioritization.”
But at the roundtable, Gawande was just another being wanting to belong. Struck by his humility and humanity, I purchased his book.
Then I discovered my father had the same widely metastatic cancer as one of the physician's first patients.
“His oncologists, radiation therapists, surgeons, and other doctors had all seen him through months of treatments for a problem that they knew could not be cured,” I had read in the Being Mortal introduction. “We could never bring ourselves to discuss the larger truth about his condition or the ultimate limits of our capabilities, let alone what might matter most to him as he neared the end of his life.
“If he was pursuing a delusion, so were we. Here he was in the hospital, partially paralyzed from a cancer that had spread throughout his body. The chances that he could return to anything like the life he had even a few weeks earlier were zero.
“But admitting this and helping him cope with it seemed beyond us. We offered no acknowledgment or comfort or guidance. We just had another treatment he could undergo. Maybe something very good would result.”
That's when I closed the book. It was someone else's story, I concluded, not mine.
* * *
My hometown's Brattleboro Area Hospice thinks differently. Believing Being Mortal to hold universal truths, it sponsors periodic screenings of Gawande's supplemental PBS documentary in hopes of sparking private and public discussion.
“It's an uphill slog at times because people don't want to talk about it,” Hospice Program Coordinator Patty Dunn said when I stopped by - professionally, not personally, I stressed - upon returning from the roundtable.
“We live in a health-care system that's about pulling out all the stops, yet there comes a point where treatments are futile,” she continued. “If people were to think about the end of life, they would realize they have certain wants.”
“In order for those to play out, you have to talk about it, write things down, and pick someone who can advocate for you.”
* * *
But my family wasn't thinking of any of that when my 80-year-old father complained of back pain in June 2017. We figured he simply had to stop attempting so much yard work.
A doctor instead diagnosed the problem as prostate cancer - the type we believed a few rounds of chemotherapy and radiation could contain.
That August, my father joined three generations of family in touring Ireland.
That September, he could barely move out of his chair.
The new plan called for physical therapy in a hospital that October and nursing home that November. The discovery of a broken hip that December simply sparked preparation for replacement surgery at Dartmouth-Hitchcock Medical Center in neighboring New Hampshire that January.
The second Tuesday of 2018 saw an operation - on my father's spine, which the cancer had cracked.
Wednesday, he went from trouble swallowing and trouble breathing to a collapsed lung and cardiac arrest.
Thursday, we were told to prepare for the worst.
Knowing I couldn't finish the remaining 300 pages of Being Mortal in one night, I searched the internet for the hour-long PBS synopsis.
“In medicine, when we're up against unfixable problems, we're often unready to accept that they are unfixable,” Gawande says in the program. “But I learned that it matters to people how their stories come to a close.”
“The questions that we ask one another just as human beings are important,” he continues. “What are your fears and worries for the future? What are your priorities if time becomes short? What are you willing to sacrifice, and what are you not willing to sacrifice?”
* * *
The next evening, my father woke from three days of sedation, silence, and sluggish recovery, ripped out his ventilator, and asked a nurse to call my mother.
“How are you?” she asked incredulously.
“Good,” he said, not one to waste words.
Was this a momentary end-of-life rally my medical friends often witness shortly before a patient's death? Stopping chemotherapy and starting a feeding tube had led to a rebound - as well as recognition that, with cancer seizing my father's ribs and vertebrae, this was only going to get more complicated.
The upswing continued Saturday, then Sunday, then Monday.
On Tuesday, Jan. 16, 2018, doctors called for a family meeting. It was 11 a.m. when the medical team announced it couldn't do anything more, that my father might live a couple of days, possibly a couple of weeks.
What did we want to do?
We asked to think about it over lunch.
My two sisters and I didn't eat. Instead, we joined our father in the intensive care unit. He lay agitated, trying to speak but challenged by a breathing tube. My older sister talked about our mother just outside as my younger sister turned on an Irish Tenors CD.
Our father began to relax. Then a red monitor light flashed. Without words, a nurse made clear this was the moment you see in the movies but never believe you'll ever experience.
Circling the bed, everyone held someone else's hand and repeated impromptu, round upon round of we love you and thank you and don't worry we remember everything about taking care of the house and ...
The Irish Tenors continued their serenade.
“If they sing 'Danny Boy,'” my younger sister said, “I'm going to lose it.”
She fumbled with a box of tissues, which flew out and over our father like confetti. In an instant, three grown children regressed a half century to laugh through tears while reassuring they'd pull it together, a veritable Family Circus cartoon of Not Me having flung sand all over Dad's beach blanket.
Track 11, “How Are Things in Glocca Morra?” ended as the nurse confirmed what we already knew.
Track 12, “Danny Boy,” began as we stepped outside to tell my mother.
* * *
Driving home a year ago, my family decided to wait a day before informing anyone so we could pause and plan.
But in a small town and age of social media, the phone rang as soon as we opened the door, with the news reported at the start of the 6:15 p.m. locally televised Selectboard meeting, by 7:30 p.m. on the website of the Brattleboro Reformer and by 8:30 p.m. on its 10,000-follower Facebook page.
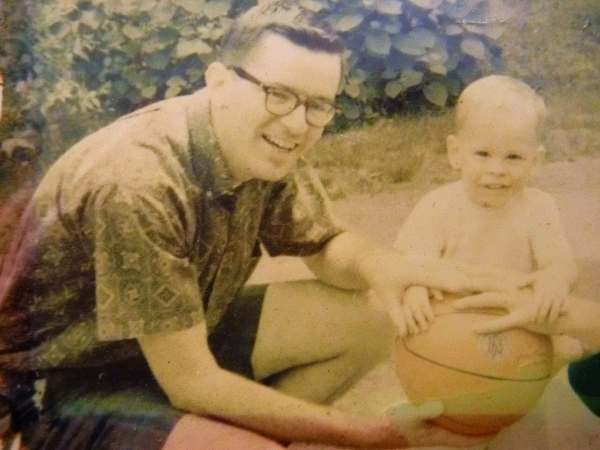
My father, Timothy O'Connor Jr., won election in 1975 as the first modern Democratic speaker of the Vermont House of Representatives. But I'll most remember the hometown headline that skipped the resume to simply report “Vermont mourns the death of 'a gentle soul.'”
I had put Being Mortal aside when Brattleboro insurance agent Ben Underhill asked how I was doing. Hearing about my Gawande meeting, Underhill talked of his rare form of blood cancer whose decade and a half of treatment had led to nerve and bone damage and the need for crutches and a wheelchair.
“I've had years to think about this,” he said.
Most people haven't. I told him I'd write this story.
Underhill died last August at age 59. I've taken too many months to start and finish it, let alone converse about end-of-life choices or consider an advance-health-care directive.
I'm not alone in my avoidance.
“Accepting that life can be shorter than we want is very difficult,” Gawande concludes. “It's easy for all of us, patients and doctors, to fall back on looking for what more we can do, regardless of what we might be sacrificing along the way. You know, people have priorities besides just living longer. You've got to ask what those priorities are.”
For in the end, Being Mortal isn't about how to die, but how to live.